The majority of gynecological cancers today can be cured, but the chances of recovery significantly depend on the stage at which the disease is diagnosed and treatment is initiated. Surgery is often part of the treatment for malignant changes, and today, a well-chosen and executed intervention by a skilled specialist offers a good chance of recovery.
The majority of gynecological cancers today can be cured, but the chances of recovery significantly depend on the stage at which the disease is diagnosed and treatment is initiated. Surgery is often part of the treatment for malignant changes, and today, a well-chosen and executed intervention by a skilled specialist offers a good chance of recovery.
Breast Cancer and Sentinel Lymph Node Surgery
During the removal of a malignant breast tumor, we also examine the so-called "sentinel" lymph nodes. For the breast, it can be fairly accurately determined which lymph nodes the tumor may spread to from a specific cancerous focus. Locating and examining the first, technically sentinel, lymph node(s) following the tumor is of great significance in determining the progress of the cancer.
The surgery is performed under anesthesia. During the operation, we make a suitably sized incision in the breast based on preliminary plans. Along with the breast tumor, we also remove the healthy tissue surrounding it. If the tumor is not palpable, we localize the precise location of the tumor by marking the area to be removed prior to surgery. This can be done in several ways: under the guidance of ultrasound or mammography, with the help of a thin wire, or by administering a small amount of radioactive marking substance.
For T1, T2, T3-sized breast tumors, when there is no proven metastasis to the axillary region, the removal of the sentinel lymph node usually occurs simultaneously with the removal of the tumor formed in the breast. A rapid microscopic pathological examination of these lymph nodes can already take place during the operation, or we send it for detailed histological examination, the result of which is one of the most important indicators of the outcome of the disease. If no cancer cells can be seen in the examined lymph nodes, we can assume that there are none in the future either. Thus, it is not necessary to remove further lymph nodes, or the entire lymph node chain, recovery is quicker, there is less pain, and the risk is lower.
Breast cancer can also be treated with total mastectomy, and all axillary lymph nodes can also be removed, depending on the stage of the condition and the individual characteristics of the patient.
Bilateral Ovarian Removal
Bilateral oophorectomy or ovariectomy is a surgical procedure in which both ovaries are removed.
In the case of confirmed ovarian cancer, or if there is a high risk of its development, the intervention is also extended to remove the fallopian tubes.
Risks of surgery
Ovariectomy is a relatively safe procedure that has a low chance of causing complications, which may include the following:
- bleeding
- infection
- damage to surrounding organs
- the disintegration of the tumor and the scattering of the released tumor cells
- retention of ovarian cells after the operation, which in the case of endometriosis, in pre-menopausal women, may cause symptoms again (e.g. pelvic, lower abdominal pain)
- ileus
In the case of removal of both ovaries – for women of childbearing age – the state of menopause immediately sets in. The reduced level of female hormones causes the symptoms in such cases:
- heat waves
- vaginal dryness
- depression
- increased tendency to heart disease
- memory impairment
- decreased libido
- osteoporosis, bone fractures
Hormone therapy can be used to treat the above symptoms, which is usually continued until the age of 50.
How to prepare for surgery?
Before the operation, your doctor can give you the following advice, the following of which can promote its success:
- drinking a laxative solution the day before surgery, which helps to clean the bowels
- on the day of surgery (or in the 8-12 hours before surgery) do not eat and limit your fluid intake
- regularly taken medications may be withdrawn or switched to other medications before and after surgery
- a detailed ultrasound and/or CT examination may be necessary in order to precisely plan the intervention
How to plan for a hospital stay?
A few days of hospitalization may be necessary after oophorectomy. The length of stay depends on the type of intervention (laparotomy, laparoscopy), its indication and the patient's general state of health. Your doctor can give you personalized information about the required length of hospitalization.
How can you prepare for possible infertility before surgery?
If you still want to have a child after the operation, consult your doctor about the possibility of this. If both ovaries are removed but the uterus remains, you can still get pregnant using assisted reproduction methods. A fertility specialist can help you with how.
Possible way of surgery:
The operation is performed under anesthesia. There are two ways to intervene:
- Traditional, open abdominal surgery (laparotomy): during a laparotomy, we make an incision in the abdominal wall to open the way to the ovaries. The surgeon separates the ovary from its supply vessels and surrounding tissue and then removes it.
- Laparoscopy, keyhole surgery: during laparoscopy, the abdominal organs can be accessed through 3 or 4 small incisions made on the abdominal wall, using special tools. The surgeon places a camera in the first hole, and the tools necessary to perform the operation in the others. With the help of these, the ovaries are separated from the blood vessels that supply them, then placed in a bag and removed through one of the small holes.
The choice of the method of surgery depends on the nature of the underlying disease. The laparoscopic method involves less post-operative pain and a shorter recovery time, but in the case of tumors, laparotomy is usually the safer procedure. Sometimes, laparoscopy can be converted to open surgery during the procedure (e.g. in the case of a large tumor or more severe bleeding during the operation).
After surgery, you can expect the following:
- we will keep him under observation until the effect of the sleeping pill wears off
- then we will place you in your room, where you will have to stay in for 24 hours to a few days, depending on the type of surgery
- during recovery, try to move and get up as soon as possible, as this promotes faster healing
- recovery time depends on the type of procedure, indication and your general condition
- on average, 6 weeks after surgery, most patients can return to their pre-surgery tasks and activities; even this time can be reduced to two weeks in case of laparoscopic intervention
Adnexectomy (salpingo-oophorectomy)
Adnexectomy or salpingo-oophorectomy is a surgical procedure involving the simultaneous removal of the ovary and fallopian tube. This procedure is most commonly performed in confirmed cases of ovarian cancer.
Malignant ovarian tumors are symptom-poor in the early stages, and their presence can only be inferred by vaginal ultrasound and blood tests for tumor markers (CA-125 and HE-4). However, for a confirmed diagnosis, we need to perform an exploratory laparotomy (so-called diagnostic abdominal incision) and analyze the results of the histological sample obtained by the freezing method, which outlines the exact course of the operation. In the case of malignant tumors, the procedure is almost exclusively performed by laparotomy. Depending on the extent of the tumor, the uterus, pelvic and abdominal lymph nodes, and a part of the peritoneum (abdominal lining) may also be removed. In the case of distant metastasis, chemotherapy and radiation may be considered as treatment alternatives, either before or after surgery.
For more detailed information about the possible indications, course, and what you need to know about the procedure, you can read about ovary removal.
Para-aortic Block Dissection
Advanced stages of malignant gynecological tumors (cervical cancer, endometrial/uterine cancer, ovarian cancer) can metastasize to the lymph nodes along the abdominal section of the aorta, the main artery. The removal of these metastases and the tumor organ can be the basis for healing. Paraaortic block dissection and the removal of the tumor-initiating organ are performed simultaneously, within the same surgical framework. For detailed information on how the operation is performed, you can read here in the section about hysterectomy, and in the section on ovary removal on this page.
Complex Gynecological Surgeries
Complex gynecological surgeries refer to those procedures - mostly necessitated for oncological reasons - that involve simultaneous intervention on multiple organs, possibly spanning multiple specialties. In cases of cancer, multiple female reproductive organs can be affected, necessitating, for example, the simultaneous partial removal of the ovaries, fallopian tubes, and uterus. Moreover, alongside the gynecological primary disease, the digestive tract or the urinary bladder and ureters might also be involved, meaning that the operating surgeon must also be familiar with the surgery of these border areas.
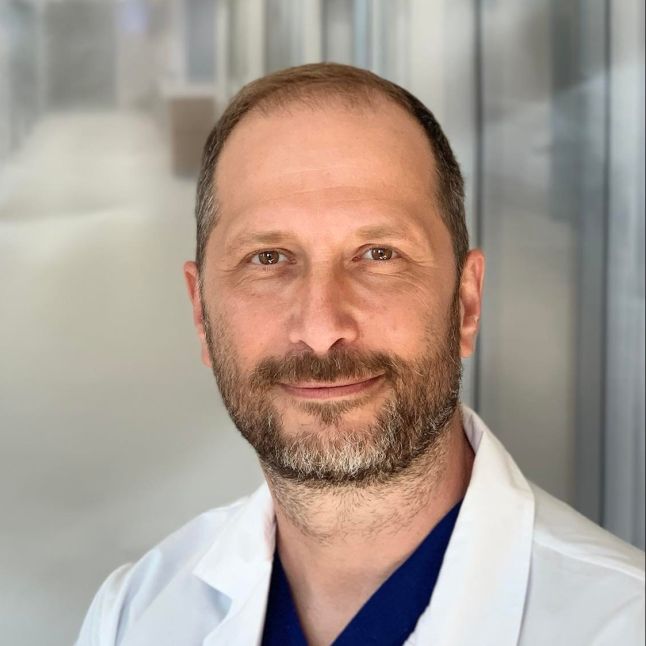
Our gynecological surgeons who perform complex surgeries have considerable professional preparation and experience. They carry out even the most challenging interventions using the most advanced equipment and hospital background.
-
Bilateral removal of ovariesFrom 910 000 Ft
-
Melanoma/mastectomy excision + sentinelFrom 1 041 000 Ft
-
Para-aortic block dissectionFrom 1 527 000 Ft
-
Unilateral salpingo-oophorectomyFrom 766 500 Ft